Allergies are among the most common chronic health issues affecting people around the world, with dust allergies being one of the most prevalent. Many individuals experience constant sneezing, nasal congestion, or itchy eyes without realizing that the source could be nearby, such as in their bed, couch, or carpet. If you notice that you feel worse indoors than outdoors, there’s a good chance you may be dealing with a dust allergy.
This article will explore what a dust allergy is, its causes, symptoms, treatments, and prevention strategies, providing you with the information you need to manage it effectively.
1. What is a Dust Allergy?
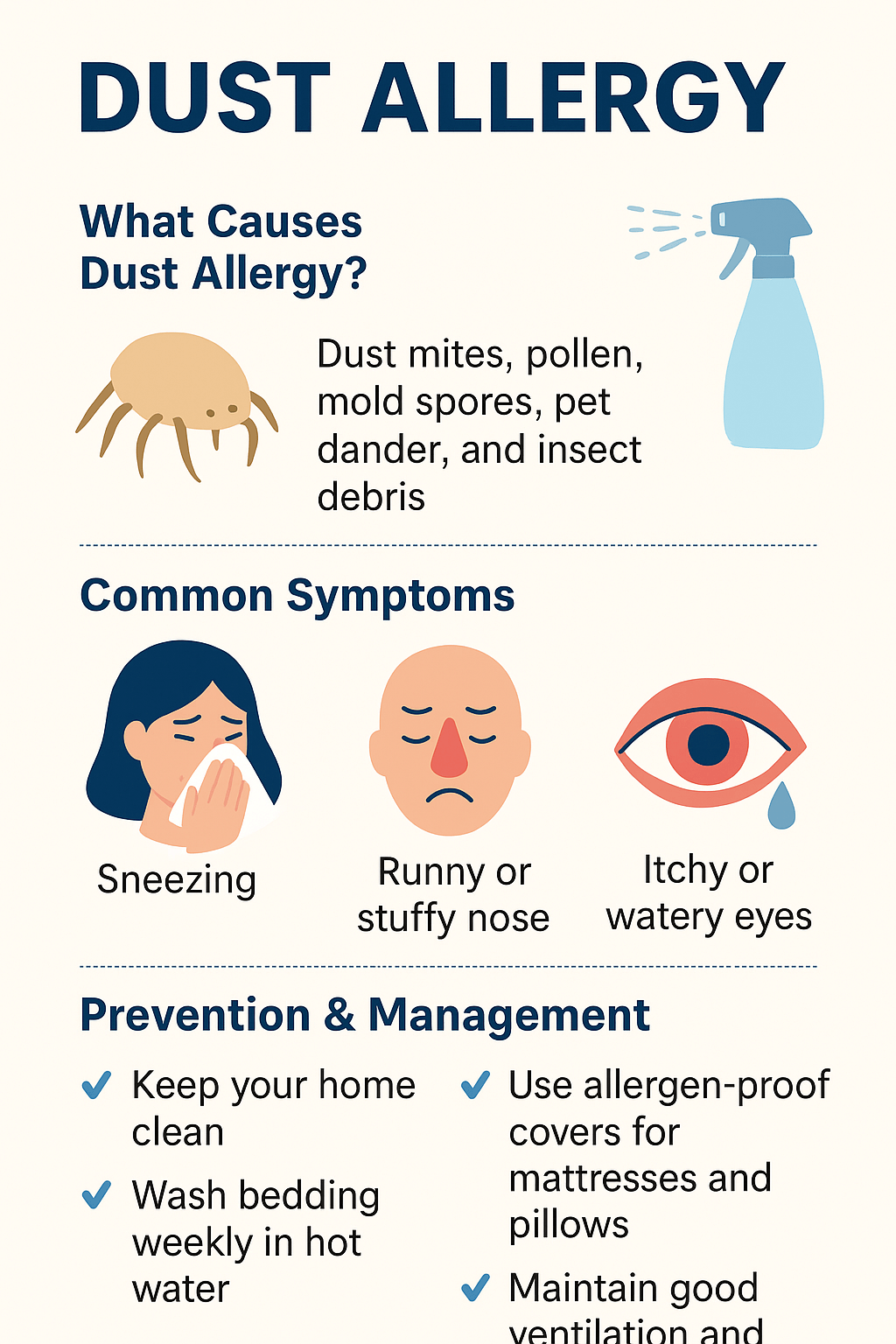
A dust allergy is the body’s immune system overreaction to substances found in household dust. Dust is not a single material; it’s a mix of tiny particles that can trigger allergic reactions in sensitive people. The most common triggers are:
- Dust mites: Microscopic organisms that thrive in warm, humid environments such as bedding, upholstery, carpets, and curtains. They feed on dead human skin cells and are the leading cause of dust allergies.
- Pollen: Outdoor allergens like tree or grass pollen can settle inside homes and mix with dust.
- Mold spores: Damp environments allow mold to grow, releasing spores that attach to dust particles.
- Pet dander: Tiny flakes of skin, hair, and saliva from cats, dogs, or other animals often get trapped in household dust.
- Insect debris: Remnants from cockroaches and other insects can also act as allergens.
When people with dust allergies inhale these particles, their immune system mistakes them for harmful invaders and releases chemicals such as histamine, leading to allergic symptoms.
2. Symptoms of Dust Allergy
Dust allergy symptoms frequently resemble those of hay fever or the common cold, which can make diagnosis challenging. However, unlike a cold, allergy symptoms do not resolve within a few days; they continue as long as the person remains exposed to allergens.
Common symptoms include:
- Frequent sneezing, often in bursts
- Runny or stuffy nose (nasal congestion)
- Itchy, red, or watery eyes
- Coughing or wheezing, especially at night or early morning
- Postnasal drip, where mucus drips down the throat
- Itchy throat, nose, or skin
- Worsening asthma symptoms (shortness of breath, tight chest, wheezing)
Children may also show signs such as frequent rubbing of the nose or eyes, disrupted sleep, and irritability due to nasal blockage.
3. Risk Factors
Not everyone develops a dust allergy, but certain factors increase the risk:
- Family history of allergies, asthma, or eczema
- Living in humid environments, which encourage dust mite growth
- Exposure to pets in the household
- Cluttered or carpeted homes, where dust accumulates easily
- Weak immune system or early childhood exposure to allergens
4. Complications of Dust Allergy
If left untreated, dust allergy can lead to more severe health issues, including:
- Asthma flare-ups: Dust mites are a leading trigger for asthma.
- Chronic sinusitis: Constant nasal congestion can cause sinus infections.
- Poor sleep quality: Nighttime allergies disrupt rest, leading to fatigue.
- Reduced quality of life: Persistent symptoms can affect productivity and mood.
5. Diagnosis
Doctors diagnose dust allergy using a combination of medical history, physical exams, and allergy testing:
- Skin Prick Test: Small amounts of suspected allergens are applied to the skin, and any allergic reaction (redness, swelling, itching) confirms sensitivity.
- Blood Tests: These measure the level of specific antibodies (IgE) in the bloodstream in response to allergens.
Identifying the exact allergen is crucial because it helps develop an effective management plan.
6. Treatment Options
While dust allergy cannot be completely cured, various treatments can control symptoms:
a) Medications
- Antihistamines: Reduce sneezing, itching, and runny nose (e.g., loratadine, cetirizine).
- Decongestants: Relieve nasal blockage by shrinking swollen tissues (e.g., pseudoephedrine).
- Nasal corticosteroid sprays: Reduce inflammation in nasal passages (e.g., fluticasone, mometasone).
- Leukotriene inhibitors: Block inflammatory chemicals (used in asthma and severe allergies).
b) Allergy Shots (Immunotherapy)
For long-term relief, allergists may recommend allergy shots, which gradually desensitize the body to allergens by injecting increasing amounts over time.
c) Sublingual Immunotherapy (SLIT)
Instead of injections, allergen tablets are placed under the tongue to help the immune system build tolerance.
d) Asthma Medications
If asthma is triggered by dust allergies, inhalers (bronchodilators or corticosteroids) may be prescribed.
7. Prevention and Management
The most effective way to manage dust allergy is by minimizing exposure. Here are practical strategies:
Home Cleaning
- Vacuum floors and furniture twice a week using a HEPA filter vacuum.
- Dust surfaces with a damp cloth to prevent allergens from becoming airborne.
- Wash bedding and pillowcases weekly in hot water (at least 60°C/140°F).
- Reduce clutter, stuffed toys, and unnecessary fabrics that collect dust.
Bedroom Precautions
- Use allergen-proof covers on mattresses, pillows, and duvets.
- Replace pillows every 1–2 years.
- Avoid heavy curtains and opt for washable blinds.
- Keep humidity levels below 50% with a dehumidifier.
Air Quality
- Use air purifiers with HEPA filters to reduce dust mites and allergens.
- Maintain proper ventilation but avoid letting in outdoor pollutants during pollen season.
- Avoid smoking indoors, as it worsens allergy symptoms.
Lifestyle Adjustments
- Bathe pets regularly and limit their access to bedrooms.
- Remove carpets if possible, especially in bedrooms.
- If allergic symptoms are severe, consider professional cleaning services.
8. Living with Dust Allergy
While managing dust allergy requires effort, it is possible to live comfortably with the right adjustments. Key steps include:
- Monitoring symptoms and keeping track of triggers
- Following a treatment plan prescribed by an allergist
- Maintaining consistency in cleaning and preventive measures
- Seeking medical advice early if symptoms worsen or asthma develops
By adopting these habits, people with dust allergy can significantly reduce flare-ups and enjoy a better quality of life.
9. When to See a Doctor
Consult a healthcare professional if:
- Symptoms interfere with daily activities or sleep
- Over-the-counter medications are not effective
- You have frequent asthma attacks triggered by dust
- You experience chronic sinus infections
Early intervention prevents complications and helps tailor an effective long-term management plan.
Conclusion
Dust allergies might appear as a minor issue, but for many individuals, they can disrupt daily life and have long-term health consequences. It is essential to understand the causes, recognize the symptoms, and implement preventive measures to manage dust allergies effectively. While completely eliminating dust is impossible, you can significantly reduce its impact by maintaining regular cleaning routines, making smart adjustments in your home, and seeking appropriate medical treatment.

